An ultra-minimally invasive form of surgical treatment for cervical, thoracic and lumbar herniated disc, sciatica(radiculopathy) , spinal stenosis, cervical radiculopathy and/or myelopathy and other spinal conditions leading to pain and disability
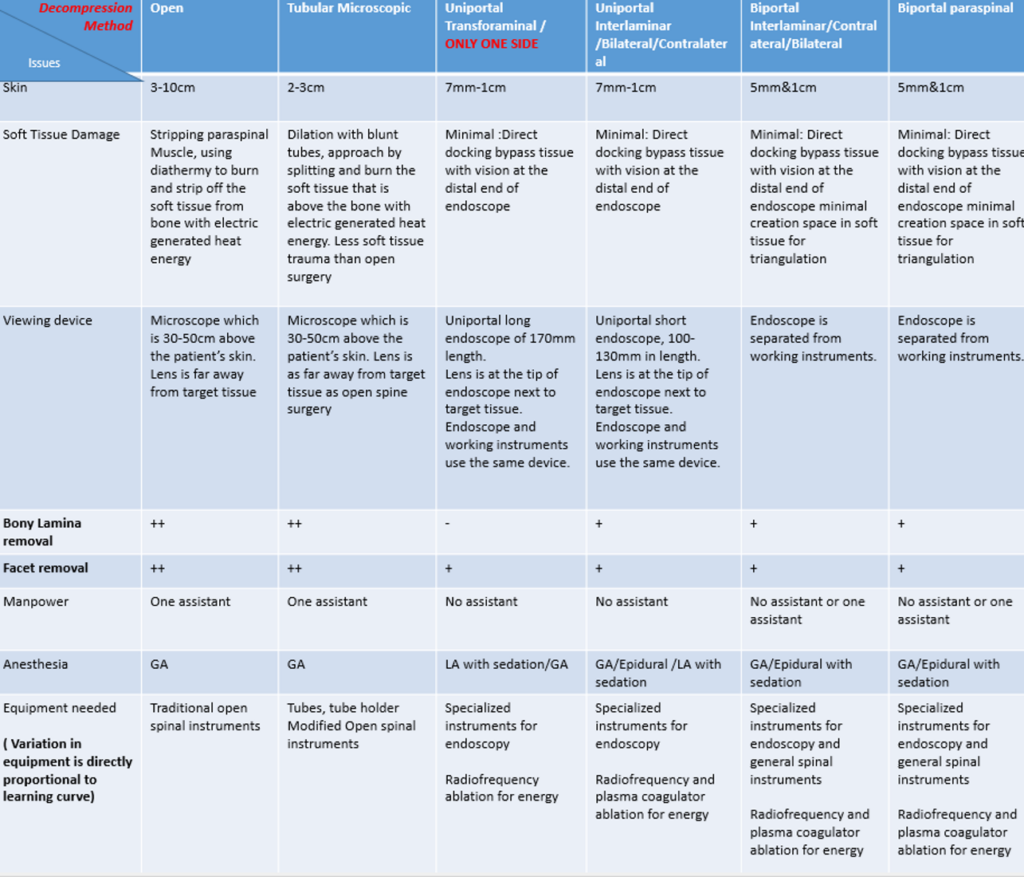
What is the difference in terms of technology between open spinal surgery, minimally invasive microscopic and endoscopic spinal surgery
Spinal surgery is offered to patients when patients have unstable spine, compression of nerves and/or deformity of the spine. Patients who have such problems in spine presents with neck/back pain, limbs pain and nerve symptoms such as weakness, numbness , unstable walking , hands cannot function as per normal and /or bladder/bowel problems. Spinal surgeries when performed open typically involves making a 3-10cm cut in the skin, muscles are split apart and burnt with electric generated heat energy (diathermy) and traditional spinal instruments to expose underlying bone and ligaments which are removed to create space around spinal nerves (Decompression). As bones, joints and ligaments are cut or patient has inherent unstable spine, screws and cage are inserted to stabilize the spine in some cases (fusion). Open spinal procedures can be done with naked eyes, microscope or loupes magnification [1].
The use of endoscope in medicine is not a new concept. Currently, endoscope is widely used and has replaced the traditional open surgery in several general surgical, neurosurgical and orthopaedic surgeries. For example, many sports related injuries are treated with knee arthroscopy rather than open knee repair of torn ligaments. Similarly, when one has a polyp in colon for biopsy, a colonoscopy is performed to remove the poly or biopsy it. Spine surgery is one of the latest subspecialty in Orthopaedic and Neurosurgery which uses endoscope to treat its various conditions.
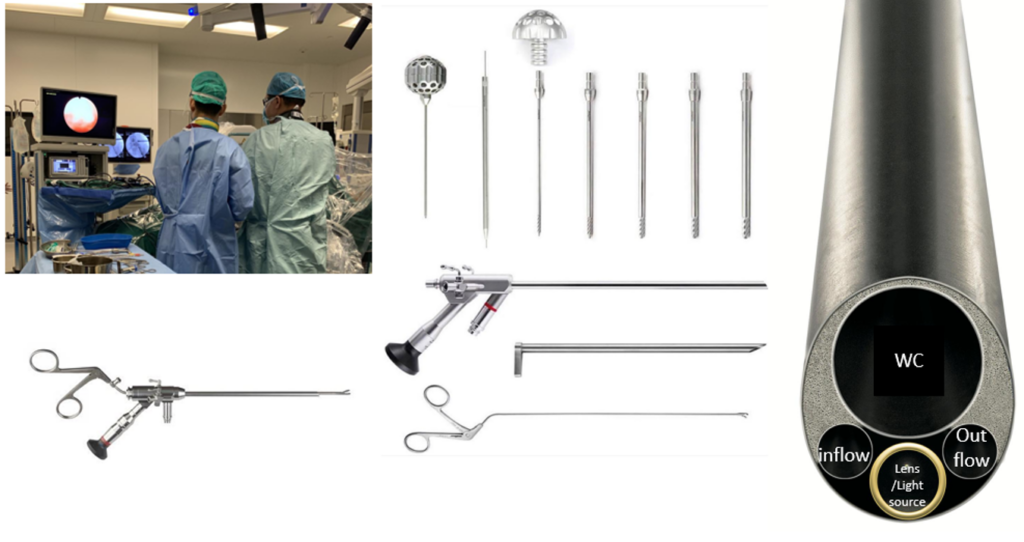
Endoscopic spine surgery is one of the least invasive version of minimally invasive spine surgery. Some surgeons term it as the bridge between pain procedure and minimally invasive open spinal surgery. (Figure 1)
It involves the use of an endoscope which is a 8-10mm in diameter with 4 functions:
1) Irrigation- the inflow of saline from inflow port constantly washout tissue and blood clots that is required to be removed.
2) Magnification by lens- to improve safety and to visualize nervous tissue clearly.
3) Light source- to provide clear visualization.
4) Working channel – delicate endoscopic instruments can be passed into a small working channel in an endoscope to reach the target disc, bone, nerve region to perform surgery.
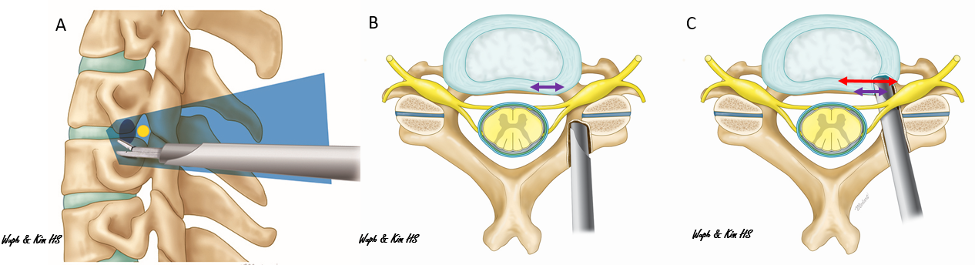
Together with enhancement of specialized working instruments and usage of constant inflow and outflow of normal saline into one device is used to reach target site of spinal nerves bypassing the burning and cutting of soft tissues. One or two subcentimeter (7mm-1cm) skin incision is usually all it required to complete the surgery. As the lens is in the front of the endoscope, surgeon does not need to burn all the tissue from the level of skin to bone in order to reach the target site. Surgeon can place endoscope directly to target site by blunt dilation of the soft tissue hence it will decrease pain, blood loss and chance of soft tissue trauma and infection. As it is a sophisticated form of spinal surgery, specialized training and courses are required in order for accreditation to perform such surgery effectively. Latest evidence in literature of endoscopic spine surgery shows good results, safety profile, less blood loss, less infection rate, excellent wound healing, less scars, less back pain and societal cost effectiveness when compared to open spinal surgery[2-4].
What is the difference between endoscopic spine surgery and minimally invasive spine surgery?
Minimally invasive spinal surgery is similar to open spinal surgery in terms of using microscope, diathermy and traditional spinal instruments, however using tube dilation and some specialize devices, muscles can be split rather than burnt and smaller incision is made on the skin. Microscope is placed 30-50cm above the patient in both types of surgery hence tissues from skin to the spinal bone target must be removed /burnt /split so that the surgeon can see clearly through the microscope to decompress spine.
In endoscopic spine surgery, the operation is performed under irrigation. This involves 3 aspects: 1) lens and light can see under normal saline conditions to visualize directly at the target site deep in the spinal canal and not 30-50cm above the skin, 2) constant washing of debris and cooled heat generated during surgery. This decreases charring of soft tissue and inadvertent damage of soft tissue and lower risk of infection. 3) Instruments are passed directly to the target site without traumatizing.
Minimally invasive spine surgery generally required general anesthesia to complete the surgery. Endoscopic spine surgery can be performed under local anesthesia with sedation in selected cases. It can be performed with epidural anesthesia and general anesthesia as well. In some patients who have poor cardiac reserved and cannot undergo general anesthesia, it is good to discuss the surgical options with an endoscopic spine surgeon to assess whether the decompressive surgery can be performed under local anesthesia with sedation. (Table 1)
There is evidence that patients who had undergone endoscopic spine surgery generally will have a shorter hospital stay, less postoperative pain, less blood loss and smaller scar than minimally invasive spine surgery and open spinal surgery[3, 5, 6]. In our experience, most of our patients in our series who underwent endoscopic decompression stayed in hospital for less than 23hours[2]. As a result, we tend to do 1-3 level endoscopic spinal decompression as day surgery.
What are the conditions suitable for endoscopic spine surgery?
With the evolution of endoscopic spine surgery, endoscopic spine surgery indications have been extended to many areas of spine[7]. Dr. Wu have performed and published the endoscopic technique and its application in lumbar spine:
Herniated disc is a condition that occurs when soft jelly like centre of intervertebral disc bulges or ruptures through the tough outer layer of the disc and put pressure in the nerves causing pain in the back and radiates to the buttock and the leg(s) with numbness and tingling(sciatica)
- Lumbar spinal decompression for spinal stenosis (tight spinal canal with sciatica, claudication and back pain with leg pain)[2, 10]
Spinal stenosis is a narrowing of spinal canal which put pressure on the spinal cord and nerves, causing pain, numbness, weakness and pins and needles feeling in arms and legs. Severe cases may present with bladder and bowel problems.
Degeneration of the disc and wearing out of the spine joints lead to instability of the spinal segment which can slipped forward, backward or sideway leading to spondylolisthesis.
- Chronic lower back pain treatment for osteoarthritis /spondylosis /degenerated disc disease. [13, 14]
With degeneration of disc and facet joints, osteoarthritis and spondylosis wearing out of the joints occur leads to chronic pain due to activation of the painful pathway. Endoscopy can target specific nerve fibres as pain management.
Due to incongruence and loading of spine in asymmetrical manners, scoliosis and spondylolisthesis may occur, in some selected curves and deformity, Dr. Wu can correct the deformity with endoscopic scoliosis correction.
In Cervical Spine and Thoracic Spine
- Decompression( foraminotomy) for prolapsed disc and tightness in spine leading to arm pain , myelopathy [17, 18]
- Ossified ligamentum flavum [19-21]
- Tumor surgery removal[19, 22]
- Thoracic decompression for prolapsed disc, myelopathy, ossified ligamentum flavum [9, 20]
Generally, in expert hands, endoscopic spine surgery can be performed in nearly 80-90% of conditions which required spinal surgery. Many of this form of surgery can be done in outpatient/ambulatory settings or as a short stay in hospital. Our centre is not advocating that all spine conditions should always be treated with spinal endoscopy, in fact our endoscopic spine surgeon is experienced and had undergone extensive training with several fellowships in open spinal surgery, deformity correction, scoliosis correction as well as tumor resection surgery through approaches from the back, the front and the side. It is in the best interest for the patients to understand all treatment options available and decide which most suitable option is after weighing the benefits and risks.
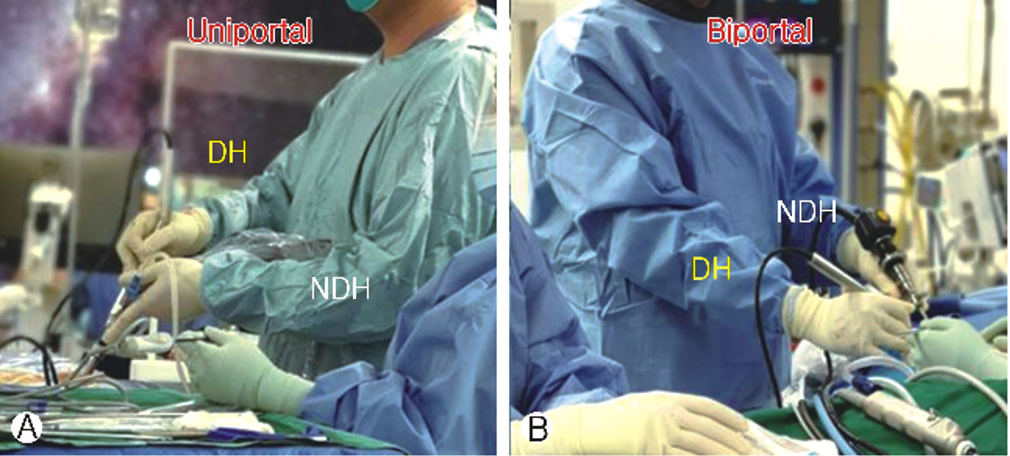
One port endoscope (Figure 2a) or two ports endoscopic procedures ( Figure 2b) can also be used to fit in the natural window use of midline lower back used in traditional spine surgery with one or two subcentimeter incisions to perform more complex procedure such as revision spinal canal decompression, interbody fusion procedure, washing out of infective tissue in spine, tumor procedures.
Dr. Wu Pang Hung has established a protocol to perform day surgeries for patients who presented with sciatica (herniated disc /prolapsed intervertebral disc), spinal stenosis, and cervical radiculopathy and in selected cervical and thoracic myelopathy patients with endoscopic spine surgery in Singapore and advised given to overseas centres to set up their practice. Here are some of the references of articles he wrote which described these procedures [2, 13, 17, 22, 23].

![Figure 4: Biportal Cervical Endoscopic Decompression and resection of a benign osteochondroma. Figure 4 obtained from publication by Wu et al[25]](https://khmermedical.com/wp-content/uploads/2024/05/Picture3-1024x924.png)
![Figure 6: Post-operative Radiological Investigation and Picture showed the skin incision scars. Fig. 5A and B showed lateral and anteroposterior view of lumbar XR showed good positioning of the interbody cage and implants. Fig. 5C: showed 4 incisions required for 4 pedicle screws placement, the right upper incision was also used for endoscope working channel for Endo-TLIF. Fig. 5D: Coronal mid body CT scan showed good placement of bone graft and intebody cage. Fig. 5E: Midsagittal cut CT scan showing reduction of spondylolisthesis with good placement of cage and bone graft. Fig. 5F: Axial cut CT scan showing good oblique position of the cage. Figure reproduced from Kim and Wu et al[15]](https://khmermedical.com/wp-content/uploads/2024/05/Picture5.png)
What are the types of endoscopic spine surgery (Endoscopic Spine Surgery procedure)
Endoscopic spine surgery is divided into uniportal and biportal endoscopic spine surgery[26]. Due to evolution of endoscopic spine surgical technique, more and more conditions can be treated endoscopically as a day procedure.
In Achieve Spine and Orthopaedic Centre, we can convert up to 80% of our load of traditional open spinal surgery to endoscopic spine surgery. In selected cases, they can be performed as outpatient day surgery centre procedures. As learning curve of spinal endoscopy is steep, patient needs to speak to spinal surgeon to decide whether he/she is suitable for endoscopic spine surgery in their practice.
Here is the table according to the region of the body and the common description of the endoscopic spine surgery. Those highlighted in red can be performed under local anesthesia
Lumbar :
Anatomy( indications) | Uniportal | Biportal |
Extraforamen ( Prolapsed disc, Bertolotti syndrome, adjustment of interbody cages) | Extraforaminal endoscopic lumbar discectomy (EELD) | Far lateral approach/ paraspinal approach unilateral biportal endoscopy
|
Foramen( Prolapsed disc, foraminal stenosis , adjustment of interbody cages) | Transforaminal endoscopic lumbar discectomy ( TELD)
| Far lateral approach/ paraspinal approach unilateral biportal endoscopy |
Lateral Recess ( spinal stenosis, adjacent segment degeneration, prolapsed disc, facet cyst, discal cyst) | Transforaminal endoscopic lateral recess decompression (TELRD) Lumbar endoscopic lateral recess decompression ( LELRD) | Unilateral Biportal Endoscopic interlaminar approach ( UBE)
|
Central Canal with or without contralateral lateral recess( spinal stenosis, adjacent segment degeneration, prolapsed disc, facet cyst, discal cyst) | Lumbar endoscopic unilateral laminotomy with bilateral decompression ( LEULBD)
Interlaminar Contralateral Endoscopic Lumbar Foraminotomy (ICELF)
| Unilateral Biportal Endoscopic interlaminar approach ( UBE) |
Interbody Fusion | Uniportal Posterolateral endoscopic interbody fusion
| Biportal posterolateral endoscopic lumbar interbody fusion
|
Others ( for advanced level surgery) | Tumor resection, infection and debridement
| Tumor resection , infection and debridement UBE assisted fusion and/or osteotomy in deformity correction |
Thoracic
Anatomy | Uniportal | Biportal |
Foramen ( prolapsed disc, calcified disc) | Transforaminal endoscopic thoracic discectomy ( TETD)
| Far lateral approach/ paraspinal approach unilateral biportal endoscopy to thoracic spine |
Lateral Recess ( ossified ligamentum flavum/ossified yellow ligament), ossified posterior longitudinal ligament | Transforaminal endoscopic thoracic lateral recess decompression (TETRD) Thoracic endoscopic lateral recess decompression ( TELRD) | Unilateral Biportal Endoscopic interlaminar approach ( UBE) to thoracic spine |
Central Canal with or without contralateral lateral recess( ossified ligamentum flavum/ossified yellow ligament), ossified posterior longitudinal ligament | Thoracic endoscopic unilateral laminotomy with bilateral decompression ( TEULBD) | Unilateral Biportal Endoscopic interlaminar approach ( UBE) to thoracic spine |
Others ( for advanced level surgery) | Tumor resection, infection and debridement with or without percutaneous screw fixation | Tumor resection, infection and debridement UBE assisted , with or without percutaneous screw fixation |
Cervical
Anatomy | Uniportal | Biportal |
Foramen and Lateral Recess ( prolapsed intervertebral disc, ossified ligamentum flavum/ossified yellow ligament), ossified posterior longitudinal ligament | Posterior endoscopic cervical foraminotomy Posterior endoscopic cervical discectomy
| Unilateral Biportal Endoscopic interlaminar approach ( UBE) to cervical spine
|
Central Canal with or without contralateral lateral recess( ossified ligamentum flavum/ossified yellow ligament), ossified posterior longitudinal ligament | Cervical endoscopic unilateral laminotomy with bilateral decompression ( CEULBD) | Unilateral Biportal Endoscopic interlaminar approach ( UBE) to cervical spine with bilateral decompression |
Others ( for advanced level surgery) | Tumor resection, infection and debridement | Tumor resection ,infection and debridement
|
What are the procedure details?
Depending on the nature of the operation and complexity, the procedures detailed will be discussed with the patient. Generally a local anesthetic /general anesthesia is applied to relieve pain during procedure and keep patient relatively sedated/ asleep to make the procedure comfortable. Patient is positioned face down, one or two 7mm incision is made on the skin to introduce endoscope into the patient’s target site. Specialized endoscopic designed equipment are used to remove the thickened ligament, excess bone spurs, and prolapsed /protruding disc that is pressing on spinal nerves. Nerve is carefully inspected during the procedure and nerve is being check again upon completion of surgery to be free of compression.
When endoscopic fusion is performed, in addition of the above, disc space is prepared under direct endoscopic visualization and cage is inserted under endoscopic visualization before putting in percutaneous screw fixation.
Where is Achieve Spine And Orthopaedic Centre?
Achieve Spine And Orthopaedic Centre (ASOC) is the first private Spine and Orthopaedic Centre in Singapore to offer full range of both uniportal and biportal endoscopic spine surgery options for treatment of various simple to complex cervical, thoracic, lumbar spinal conditions in addition to traditional open and minimally invasive microscopic spine surgery.
Its doctors are renowned Orthopaedic specialist who is experienced in the latest minimally invasive and endoscopic spine surgery techniques with focus on quick recovery and ambulatory orthopaedic and spine surgery. ASOC manages patients with all kinds of spine and orthopaedic conditions.
Achieve Spine And Orthopaedic Centre’s motto is small is beautiful, less is more, motion conservation is key.
Achieves Spine and Orthopaedic Centre is located in Mount Elizabeth Hospital, #16-11, Singapore 228510
Endoscopic Spine Surgery Recovery time
Wu et al compared his early series of uniportal and biportal endoscopic spine surgery result during his learning curve period and found the average length of stay for 90% of his patients are within 23 hours[2]. The quick recovery allows patients to walk within hours after surgery and typically does not require urinary catherization and calf pump. Many endoscopic spine patients can go home within 6 -8 hours of surgery[2].
Endoscopic Spine Surgery success rate at long term
Success of endoscopic spine surgery is comparable to open surgery in terms of long term pain relief, some of the conditions such as thoracic prolapsed disc [9, 19] which typically required open chest approach, resection of bone and perhaps screws fixation as well as lumbar foraminal pathologies[27] which required decompression and/or fusion procedure[11, 12]. These procedures can be performed with endoscopy as day surgery in selected cases with the benefits listed above. Endoscopic spine surgery is a sub specialization of spine surgery with significant learning curve and accreditation process [24, 28]. Dr. Wu Pang Hung taught in different regions around the world to promote the use of endoscopic spine surgery as a sub specialization to help surgeons in different countries to overcome their learning curve in spinal endoscopy (Figure 7) .It is in best interest for the patient to speak to endoscopic spine surgeon to discuss whether your conditions can be treated with spinal endoscopy.


- Is Endoscopic Spine Surgery Safe – Recent systematic review and metanalysis of large pool of data studies shows endoscopic spine surgery is safe and effective.
- Can endoscopic spine surgery be an alternative to artificial disc replacement? Both artificial disc replacement and endoscopic spine surgery aims to preserve motion to avoid adjacent segment disease in fusion procedures. While endoscopic spine surgery can potentially avoid the use of implants in cervical spine and some of the indication for artificial disc replacement overlaps with endoscopic spine surgery it is best to discuss with an experienced endoscopic spine surgeon on whether it is possible alternative treatment for artificial disc replacement (ADR) and anterior cervical decompression and fusion (ACDF) procedure.
References
- Fehlings, M. G.; Tetreault, L.; Nater, A.; Choma, T.; Harrop, J.; Mroz, T.; Santaguida, C.; Smith, J. S., The Aging of the Global Population: The Changing Epidemiology of Disease and Spinal Disorders. Neurosurgery 2015, 77 Suppl 4, S1-5.
- Wu, P. H.; Chin, B. Z. J., Ambulatory uniportal versus biportal endoscopic unilateral laminotomy with bilateral decompression for lumbar spinal stenosis-cohort study using a prospective registry. 2023.
- McGrath, L. B.; White-Dzuro, G. A.; Hofstetter, C. P., Comparison of clinical outcomes following minimally invasive or lumbar endoscopic unilateral laminotomy for bilateral decompression. J Neurosurg Spine 2019, 1-9.
- Gadjradj, P. S.; Broulikova, H. M.; van Dongen, J. M.; Rubinstein, S. M.; Depauw, P. R.; Vleggeert, C.; Seiger, A.; Peul, W. C.; van Susante, J. L.; van Tulder, M. W.; Harhangi, B. S., Cost-effectiveness of full endoscopic versus open discectomy for sciatica. British journal of sports medicine 2022, 56, (18), 1018-25.
- Phan, K.; Xu, J.; Schultz, K.; Alvi, M. A.; Lu, V. M.; Kerezoudis, P.; Maloney, P. R.; Murphy, M. E.; Mobbs, R. J.; Bydon, M., Full-endoscopic versus micro-endoscopic and open discectomy: A systematic review and meta-analysis of outcomes and complications. Clinical neurology and neurosurgery 2017, 154, 1-12.
- Feng, F.; Xu, Q.; Yan, F.; Xie, Y.; Deng, Z.; Hu, C.; Zhu, X.; Cai, L., Comparison of 7 Surgical Interventions for Lumbar Disc Herniation: A Network Meta-analysis. Pain physician U6 – ctx_ver=Z39.88-2004&ctx_enc=info%3Aofi%2Fenc%3AUTF-8&rfr_id=info%3Asid%2Fsummon.serialssolutions.com&rft_val_fmt=info%3Aofi%2Ffmt%3Akev%3Amtx%3Ajournal&rft.genre=article&rft.atitle=Comparison+of+7+Surgical+Interventions+for+Lumbar+Disc+Herniation%3A+A+Network+Meta analysis&rft.jtitle=Pain+physician&rft.au=Feng%2C+Fan&rft.au=Xu%2C+Qianqian&rft.au=Yan%2C+Feifei&rft.au=Xie%2C+Yuanlong&rft.date=2017-09-01&rft.eissn=2150-1149&rft.volume=20&rft.issue=6&rft.spage=E863&rft_id=info%3Apmid%2F28934804&rft.externalDocID=28934804¶mdict=en-US U7 – Journal Article 2017, 20, (6), E863.
- Kim, H. S.; Wu, P. H.; Jang, I.-T., Current and Future of Endoscopic Spine Surgery: What are the Common Procedures we Have Now and What Lies Ahead? World Neurosurgery 2020, 140, 642-653.
- Wu, P. H.; Kim, H. S.; Jang, I.-T., A Narrative Review of Development of Full-Endoscopic Lumbar Spine Surgery. Neurospine 2020, 17, (Suppl 1), S20-S33.
- Wu, P. H.; Kim, H. S.; Raorane, H. D.; Heo, D. H.; Yi, Y. J.; Yang, K.-H.; Jang, I.-T., Safe Extraforaminal Docking and Floating Technique in Transforaminal Endoscopic Discectomy for Thoracolumbar Junction for Calcified Disc Herniation: A Case Report and Technical Review Junction for Calcified Disc Herniation. J Minim Invasive Spine Surg Tech 2020, 5, (1), 26-30.
- Kim, H.-S.; Wu, P. H.; Jang, I.-T., Lumbar Endoscopic Unilateral Laminotomy for Bilateral Decompression Outside-In Approach: A Proctorship Guideline With 12 Steps of Effectiveness and Safety. Neurospine 2020, 17, (Suppl 1), S99-S109.
- Wu, P. H.; Kim, H. S.; An, J. W.; Kim, M.; Lee, I.; Park, J. S.; Lee, J. H.; Kang, S.; Lee, J.; Yi, Y.; Lee, J. H.; Park, J. H.; Lim, J. H.; Jang, I.-T., Prospective Cohort Study with a 2-Year Follow-up of Clinical Results, Fusion rate, and Muscle Bulk for Uniportal Full Endoscopic Posterolateral Transforaminal Lumbar Interbody Fusion. Asian Spine J 2023, 0.
- Kim, H.-S.; Wu, P.-H.; An, J.-W.; Lee, Y.-J.; Lee, J.-H.; Kim, M.-H.; Lee, I.; Park, J.-S.; Lee, J.-H.; Park, J.-H.; Jang, I.-T., Evaluation of Two Methods (Inside-Out/Outside-In) Inferior Articular Process Resection for Uniportal Full Endoscopic Posterolateral Transforaminal Lumbar Interbody Fusion: Technical Note. Brain sciences 2021, 11, (9), 1169.
- Wu, P. H.; Kim, H. S., Intervertebral Disc Diseases PART 2: A Review of the Current Diagnostic and Treatment Strategies for Intervertebral Disc Disease. 2020, 21, (6).
- Kim, H. S.; Wu, P. H.; Jang, I.-T., Lumbar Degenerative Disease Part 1: Anatomy and Pathophysiology of Intervertebral Discogenic Pain and Radiofrequency Ablation of Basivertebral and Sinuvertebral Nerve Treatment for Chronic Discogenic Back Pain: A Prospective Case Series and Review of Literature. International journal of molecular sciences 2020, 21, (4), 1483.
- Kim, H. S.; Wu, P. H.; Jang, I.-T., Technical note on Uniportal full endoscopic posterolateral approach transforaminal lumbar interbody fusion with reduction for grade 2 spondylolisthesis. Interdisciplinary Neurosurgery 2020, 21, 100712.
- Wu, P. H.; Kim, H. S.; Lee, Y. J.; Kim, D. H.; Lee, J. H.; Jeon, J. B.; Raorane, H. D.; Jang, I. T., Uniportal Full Endoscopic Posterolateral Transforaminal Lumbar Interbody Fusion with Endoscopic Disc Drilling Preparation Technique for Symptomatic Foraminal Stenosis Secondary to Severe Collapsed Disc Space: A Clinical and Computer Tomographic Study with Technical Note. Brain sciences 2020, 10, (6).
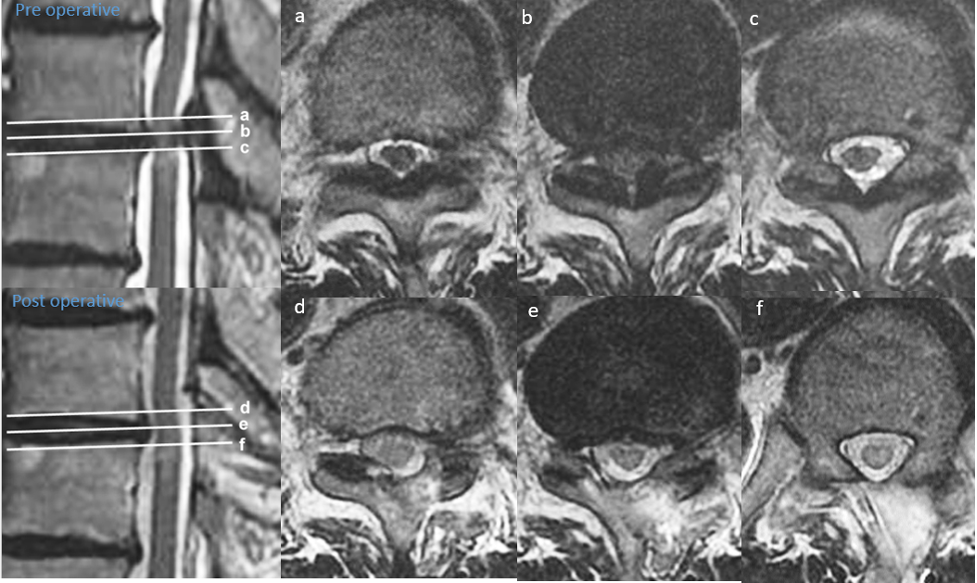
- Wu, P. H.; Kim, H. S.; Lee, Y. J.; Kim, D. H.; Lee, J. H.; Yang, K.-H.; Raorane, H. D.; Jang, I.-T., Posterior endoscopic cervical foramiotomy and discectomy: clinical and radiological computer tomography evaluation on the bony effect of decompression with 2 years follow-up. European Spine Journal 2020.
- Kim, H. S.; Wu, P. H.; Lee, Y. J.; Kim, D. H.; Kim, J. Y.; Lee, J. H.; Jeon, J. B.; Jang, I. T., Safe Route for Cervical Approach: Partial Pediculotomy , Partial Vertebrotomy Approach For Posterior Endoscopic Cervical Foraminotomy and Discectomy. World Neurosurg 2020.
- Wu, P. H.; Kim, H. S.; Kim, J.-Y.; Lee, Y. J.; Kim, D. H.; Lee, J. H.; Jeon, J. B.; Jang, I.-T., Uniportal thoracic endoscopic decompression using one block resection technique for thoracic ossified ligamentum flavum technical report. Interdisciplinary Neurosurgery 2021, 23, 100963.
- Kim, H. S.; Wu, P. H., Comparative Clinical and Radiographic Cohort Study: Uniportal Thoracic Endoscopic Laminotomy With Bilateral Decompression by Using the 1-Block Resection Technique and Thoracic Open Laminotomy With Bilateral Decompression for Thoracic Ossified Ligamentum Flavum. 2022.
- George, R.; Wu, P. H., Posterior Cervical Unilateral Biportal Endoscopic One-Block Resection Technique for Cervical Ossified Ligamentum Flavum. In Surgical Techniques Development, 2023; Vol. 12, pp 80-86.
- Hung, D. W. P.; Kavishwar, D. R. A.; Natalie, D. T. H. W.; Tan, D. G., Unilateral Biportal Endoscopic Supralaminar, Posterior Spinous Process Sparing Approach For En Bloc Cervical Laminectomy In Case Of Cervical Osteochondroma Causing Myelopathy A Case Report. North American Spine Society Journal (NASSJ) 2023, 100225.
- Lau, E. T.; Wu, P. H., Technical Note on Unilateral Biportal Lumbar Endoscopic Interbody Fusion. In Surgical Techniques Development, 2022; Vol. 11, pp 71-89.
- Wu, P. H.; Kim, H. S.; Choi, D. J.; Gamaliel, Y.-H. T., Overview of Tips in Overcoming Learning Curve in Uniportal and Biportal Endoscopic Spine Surgery. J Minim Invasive Spine Surg Tech 2021, 6, (Suppl 1), S84-S96.
- Hung, W. P.; Kavishwar, R. A.; Natalie, T. H. W.; Tan, G., Unilateral biportal endoscopic supralaminar, posterior spinous process sparing approach for en bloc cervical laminectomy in case of cervical osteochondroma causing myelopathy: A case report. North American Spine Society Journal (NASSJ) 2023, 14, 100225.
- Hofstetter, C. P.; Ahn, Y.; Choi, G.; Gibson, J. N. A.; Ruetten, S.; Zhou, Y.; Li, Z. Z.; Siepe, C. J.; Wagner, R.; Lee, J.-H.; Sairyo, K.; Choi, K. C.; Chen, C.-M.; Telfeian, A. E.; Zhang, X.; Banhot, A.; Lokhande, P. V.; Prada, N.; Shen, J.; Cortinas, F. C.; Brooks, N. P.; Van Daele, P.; Kotheeranurak, V.; Hasan, S.; Keorochana, G.; Assous, M.; Härtl, R.; Kim, J.-S., AOSpine Consensus Paper on Nomenclature for Working-Channel Endoscopic Spinal Procedures. Global spine journal 2020, 10, (2 Suppl), 111S-121S.
- Wu, P. H.; Kim, H. S.; Jang, I.-T., How I do it? Uniportal full endoscopic contralateral approach for lumbar foraminal stenosis with double crush syndrome. Acta Neurochirurgica 2020, 162, (2), 305-310.
- Wu, P. H., Early Career Challenges in Setting Up an Endoscopic Spine Surgery Practice. World Neurosurgery 2020, 144, 264-269.